
| Topic Coverage: | Neoadjuvant therapy training protocols, recovery strategies, and return-to-sport guidelines |
| Reading Time: | 15 minutes |
| Main Sections: |
• Understanding Neoadjuvant Therapy • Training Program Design • Recovery Protocols • Return to Sport Guidelines • Case Studies & Expert Tips |
| Best For: | Athletes undergoing cancer treatment, sports medicine professionals, trainers working with cancer patients |
| Key Outcomes: | Understanding how to maintain fitness during treatment, safely return to training, and optimize recovery |
Neoadjuvant Therapy-Compatible Training
Facing cancer treatment while maintaining athletic performance presents unique challenges that require a carefully structured approach to exercise and recovery. This comprehensive guide explores how athletes can maintain their fitness during neoadjuvant therapy while ensuring safe and effective training protocols.
Understanding Neoadjuvant Therapy and Athletic Performance
Let me walk you through the intricate relationship between neoadjuvant therapy and athletic performance, breaking down both the challenges and opportunities that arise during this critical treatment phase.
What is Neoadjuvant Therapy?
Neoadjuvant therapy represents a strategic medical approach where treatment is administered before the primary surgical intervention. This typically includes:
- Chemotherapy: Systematic treatment using drugs to target cancer cells
- Radiation therapy: Localized treatment using high-energy rays
- Targeted therapy: Specific treatments focusing on cancer’s molecular features
- Immunotherapy: Treatment that enhances the body’s immune response

The Athletic Performance Window
Understanding your performance window during treatment is crucial. Here’s how we’ll break this down:
Pre-Treatment Baseline
Establishing a comprehensive pre-treatment baseline serves as the foundation for developing an effective training program during neoadjuvant therapy. This process begins with a thorough fitness assessment, which includes both laboratory and field-based testing protocols.
Medical professionals and exercise specialists collaborate to evaluate cardiovascular fitness through VO2max testing, anaerobic threshold assessments, and metabolic rate measurements. These baseline metrics provide crucial data points that will guide future training modifications and help track the impact of treatment on physical performance.
Advanced Cardio Training & Muscle Density Definition
Performance testing plays a vital role in creating an objective record of the athlete’s capabilities before treatment begins. This documentation encompasses a range of performance metrics, including power output measurements, speed assessments, and sport-specific skill evaluations. The collected data helps establish realistic training goals during treatment, provides benchmarks for monitoring treatment-related changes, and offers valuable insights for healthcare providers about the athlete’s physical capabilities and limitations.

The strength and endurance benchmarking phase involves detailed assessments of both maximal strength capabilities and endurance capacity across different energy systems. Athletes undergo standardized testing protocols that evaluate their one-repetition maximums for major movement patterns, muscular endurance in sport-specific activities, and their ability to maintain power output over various time domains. This comprehensive strength and endurance profile helps identify areas that may be more susceptible to treatment-related decrements and allows for proactive programming adjustments.
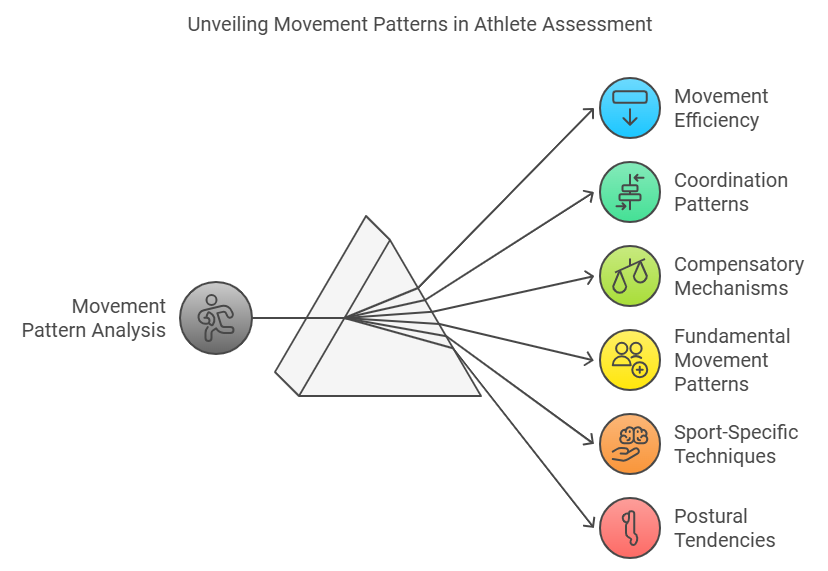
Movement pattern analysis represents the final crucial component of baseline establishment. Through sophisticated biomechanical assessments, including video analysis and potentially motion capture technology, practitioners can document the athlete’s movement efficiency, coordination patterns, and any existing compensatory mechanisms. This detailed analysis of fundamental movement patterns, sport-specific techniques, and postural tendencies provides valuable information for maintaining optimal movement quality during treatment and identifies potential areas of concern that may require additional attention or modification during the therapy period.
Treatment Phase Modifications
The implementation of adjusted training intensity zones marks a critical adaptation in the athlete’s training program during neoadjuvant therapy. Traditional training zones based on heart rate, power output, or perceived exertion must be recalibrated to account for treatment-related changes in physiological response.
This process involves regular reassessment of training thresholds, typically every 2-3 weeks, and the establishment of new “treatment-adjusted” zones that reflect the athlete’s current capabilities. These modified intensity parameters ensure that training stress remains appropriate and beneficial while avoiding excessive fatigue that could compromise treatment efficacy.
Modified volume parameters require careful consideration of both the total training load and its distribution throughout the treatment cycle.
The overall training volume typically needs to be reduced by 30-50% from pre-treatment levels, with specific adjustments based on individual tolerance and treatment schedule. This modification involves restructuring training blocks to align with treatment timing, incorporating longer recovery periods, and potentially reducing the frequency of high-intensity sessions.
The key lies in finding the optimal balance between maintaining fitness and ensuring adequate recovery capacity for treatment demands.
Adapted recovery protocols become increasingly important during treatment, as the body’s regenerative capabilities may be compromised. These protocols must be more comprehensive than standard athletic recovery methods, incorporating both physiological and psychological components.
Recovery strategies need to be synchronized with treatment timing, with particular attention paid to nutrition timing, sleep quality, and stress management. The implementation of daily monitoring systems helps track recovery status and allows for rapid adjustments when needed.
Revised performance expectations represent a crucial psychological and practical component of treatment phase modifications. Athletes and their support team must establish new, realistic performance targets that acknowledge the impact of treatment while maintaining motivation and progress. These expectations should be dynamic, allowing for both positive and negative adjustments based on individual response to treatment.
Regular reassessment of goals helps maintain athlete engagement while preventing frustration from unrealistic expectations, ultimately supporting both athletic and treatment outcomes.
Creating Your Performance Bridge
Think of maintaining athletic performance during neoadjuvant therapy as building a bridge between your pre-treatment and post-treatment fitness levels. Here’s the structural approach:
The Performance Bridge During Treatment
Performance Preservation Strategies
Let’s examine specific strategies for maintaining athletic capacity during treatment:
Timing Considerations
- Treatment scheduling optimization
- Training window identification
- Recovery period planning
- Performance testing intervals
Intensity Management
- Heart rate monitoring
- Rate of perceived exertion tracking
- Power output assessment
- Technical efficiency evaluation
100% Legal Steroids & Natural Testosterone Booster
Scientific Evidence Supporting Exercise During Treatment
Exercise Benefits During Neoadjuvant Therapy
Physiological Benefits
Performance Outcomes
Practical Implementation Framework
Here’s a systematic approach to maintaining athletic performance during neoadjuvant therapy:
Assessment Phase
- Initial medical clearance
- Performance baseline establishment
- Risk factor identification
- Goal setting and expectations
Implementation Strategy
- Progressive loading protocols
- Adaptable training schedules
- Regular monitoring systems
- Recovery optimization techniques
Monitoring and Adjustment Protocols
Establishing clear monitoring protocols is essential:
Athlete Monitoring Protocols During Treatment
Essential metrics to track during neoadjuvant therapy training for optimal performance and safety
Daily Monitoring
- Perceived fatigue levels (1-10 scale)
- Sleep quality and duration
- Resting heart rate variability
- Treatment response symptoms
- Hydration status
Weekly Assessments
- Training load tolerance
- Movement pattern quality
- Strength maintenance tests
- Cardiovascular capacity checks
- Body composition changes
Recovery Markers
- Muscle soreness mapping
- Joint mobility assessment
- Energy level tracking
- Appetite and nutrition status
- Mood and motivation levels
Performance Indicators
- Exercise capacity trends
- Technical skill maintenance
- Power output measurements
- Endurance benchmarks
- Recovery time between sets
The Path Forward
Understanding neoadjuvant therapy and athletic performance is an ongoing process that requires:
- Regular communication with medical team
- Consistent monitoring and documentation
- Flexible approach to training adaptation
- Focus on long-term athletic sustainability
By understanding these components and their interactions, athletes and their support teams can better navigate the challenges of maintaining performance during neoadjuvant therapy while ensuring safe and effective treatment outcomes.
Remember, this understanding forms the foundation for developing specific training protocols, which we’ll explore in subsequent sections of this comprehensive guide. The key is to maintain a balance between treatment efficacy and athletic performance preservation, always prioritizing long-term health outcomes while optimizing current performance capabilities.
Impact on Athletic Systems
Neoadjuvant therapy’s effect on athletic performance is multifaceted, impacting various physiological systems simultaneously. The treatment can cause significant alterations in how the body responds to exercise stimuli, requiring careful monitoring and program adjustment to maintain optimal performance levels while ensuring patient safety during the treatment phase.
Understanding these systemic changes is crucial for healthcare providers and fitness professionals working with athletes undergoing treatment. By recognizing how each system adapts and responds to therapy, practitioners can develop more effective and personalized training protocols that account for individual variations in treatment response.
These impacts necessitate a comprehensive approach to training modification, considering not just immediate performance metrics but also long-term athletic development. Regular assessment and adjustment of training programs become essential to balance the therapeutic benefits of exercise with the body’s altered capacity during treatment.
Musculoskeletal System:
During neoadjuvant therapy, athletes often experience significant changes in muscle protein synthesis, potentially leading to reduced muscle mass and strength. This decrease in protein synthesis affects the body’s ability to repair and build muscle tissue following exercise, requiring careful attention to training volume and intensity to prevent excessive breakdown.
The alteration in muscle fiber recruitment patterns presents unique challenges for maintaining technical skill and movement efficiency. Athletes may need to focus more on movement quality and neural adaptation rather than traditional progressive overload, as the body’s ability to recruit muscle fibers effectively becomes compromised during treatment.
Changes in bone density and connective tissue elasticity require special consideration in program design. Impact activities and heavy loading patterns may need modification to account for reduced structural integrity while maintaining sufficient stimulus for tissue preservation. This balance becomes crucial for long-term athletic development and injury prevention.
Cardiovascular System:
Treatment-induced changes in stroke volume and heart rate variability significantly impact an athlete’s cardiovascular response to exercise. These alterations affect the heart’s ability to efficiently pump blood, requiring careful monitoring of exercise intensity and duration to prevent overexertion while maintaining cardiovascular fitness.
Modified blood flow patterns during treatment can affect oxygen delivery to working muscles, potentially reducing exercise capacity and endurance. Athletes may experience increased fatigue at lower workloads, necessitating adjusted training zones and modified recovery periods to maintain effective cardiovascular conditioning.
The altered oxygen utilization capacity during therapy requires strategic approach to endurance training. Programs must be designed to maintain cardiovascular fitness while accounting for reduced oxygen delivery and utilization, often through shorter, more frequent sessions at appropriate intensities to prevent excessive systemic stress.
Energy Systems:
Neoadjuvant therapy significantly impacts ATP production efficiency, affecting the body’s ability to generate and sustain energy during exercise. Athletes may experience reduced power output and increased fatigue, requiring careful periodization of training intensity and volume to maintain energy system development while preventing excessive fatigue.
Modified glycogen storage capacity and altered fat utilization during treatment affect the body’s ability to fuel exercise effectively. This requires strategic nutrition timing and modified training approaches to optimize available energy stores and maintain performance capacity during both short and long-duration activities.
Changes in metabolic rate during therapy can affect recovery and adaptation to training stimuli. Athletes need carefully structured programs that account for altered energy availability and utilization, with particular attention to rest periods and nutrition strategies to support training adaptation and recovery.
Neoadjuvant therapy, which includes chemotherapy and radiation treatment before surgery, can significantly impact an athlete’s training capacity. However, research shows that maintaining an appropriate exercise routine during treatment can enhance recovery outcomes and help preserve athletic performance.
The Science Behind Exercise During Cancer Treatment
Recent studies demonstrate that properly structured exercise during neoadjuvant therapy can help mitigate treatment side effects while maintaining muscle mass and cardiovascular fitness. Similar to how muscle recovery supplements support regular training adaptation, strategic exercise during treatment helps maintain physical capacity and supports recovery.
Training Program Components
Designing Your Training Program
Cardiovascular Training
Implement moderate-intensity aerobic exercise, similar to approaches used for building muscle mass, but with appropriate modifications:
- Start with 15-20 minute sessions
- Monitor heart rate and perceived exertion
- Gradually increase duration as tolerated
- Include recovery periods between sessions
Resistance Training
Maintaining muscle mass during treatment requires special attention to recovery and progression. Consider these guidelines:
- Focus on compound movements when energy levels permit
- Adjust volume based on treatment schedule
- Incorporate natural pre-workout supplements when appropriate
- Monitor for signs of fatigue
Recovery Protocols
Recovery becomes even more crucial during treatment. Understanding how to speed up muscle recovery becomes essential for maintaining training consistency.
Safety Considerations and Monitoring
Treatment-Specific Modifications
Different types of cancer and treatments require specific modifications. For instance, patients with pectoral involvement need carefully adjusted upper body training protocols.
Recovery Optimization
Incorporating natural ingredients for improved workout recovery can support your body’s healing processes during treatment. Focus on:
- Adequate protein intake
- Anti-inflammatory foods
- Proper hydration
- Sleep optimization
Case Studies: Athletes During Treatment
Professional Cyclist
Marathon Runner
Expert Guidelines for Training Implementation
Weekly Structure
Create a flexible training schedule that accounts for:
- Treatment days (typically lower intensity)
- Recovery days (complete rest or very light activity)
- Training days (moderate activity as tolerated)
- Assessment days (monitoring progress and adjusting plans)
Exercise Selection and Progression
Consider these factors when choosing exercises:
- Current energy levels
- Treatment schedule
- Previous training experience
- Medical team recommendations
Monitoring and Adjustment Strategies
Key Metrics to Monitor During Therapy
Heart Rate Response
Track resting and exercise heart rates. Note any unusual variations from baseline.
Fatigue Levels
Monitor daily energy levels and recovery time after training sessions.
Exercise Tolerance
Track workout completion rates and perceived effort levels.
Sleep Quality
Record sleep duration and quality to optimize recovery periods.
Performance Metrics
Document strength, endurance, and skill-specific benchmarks.
Recovery Capacity
Assess time needed between sessions to feel fully recovered.
Red Flags: When to Modify Your Training
Practical Implementation Tips
Communication with Medical Team
Maintain open dialogue about:
- Exercise intentions and goals
- Current training volume
- Side effects and challenges
- Recovery progress
Documentation and Progress Tracking
Keep detailed records of:
- Training sessions
- Energy levels
- Side effects
- Performance metrics
Transitioning Back to Regular Training
Post-Treatment Considerations
After completing neoadjuvant therapy, focus on:
- Gradual increase in volume
- Progressive overload
- Technique refinement
- Building back to pre-treatment levels
Long-term Planning
- Basic Movement Patterns
- Light Resistance Training
- Cardiovascular Base
- Sport-Specific Drills
- Progressive Loading
- Technique Refinement
- Performance Training
- Competition Prep
- Full Training Load
Return to Training Timeline
Post-Neoadjuvant Therapy Training Progression
Frequently Asked Questions
Conclusion
Maintaining athletic training during neoadjuvant therapy requires careful planning, consistent monitoring, and appropriate modifications. By following these guidelines and working closely with your medical team, you can maintain a significant portion of your fitness while supporting your treatment success. Remember that every athlete’s journey is unique, and adjustments should be made based on individual response and medical guidance.
For more information about general muscle building and recovery strategies that can be adapted for your situation, visit Muscle Growth Expert.




